The entire Angolan population is at risk for malaria. In 2018 there were 3.8 million malaria cases and 16,000 malaria deaths in 2017.[1] Additionally, malaria in Angola accounts for 35% of mortality in children and 40% of pre-natal mortality.[2] Under the supervision and coordination of the National Malaria Control Program (NMCP), The MENTOR Initiative (MENTOR) in partnership with the Elimination 8 Initiative (E8), aims to strengthen malaria control in Angola.

Enter MENTOR and Elimination 8
E8 and partners aim to meet elimination targets in focus countries (Botswana, Mozambique, Namibia, South Africa, Swaziland, Zambia, and Zimbabwe) by containing cross-border transmission, promoting regional coordination and dialogue, encouraging political prioritization of malaria elimination as well as the harmonization of policies. In Angola, E8 and MENTOR in collaboration with the NMCP focus activities in the south. High transmission in southern Angola coupled with frequent migration across borders and limited access to health services has major implications for its low-burden neighbours. Thus controlling malaria transmission through effective vector control solutions is paramount to achieving reduction gains in Angola and its neighbouring countries. Thoughout 2018, MENTOR and partners were able to implement an Indoor Residual Spraying (IRS) campaign in seven southern municipalities of Angola. The goal of this campaign was to: ‘Reduce the burden of Malaria in targeted border areas of Cuando Cubango and Cunene Provinces in Angola, to aid achievement of elimination efforts in neighbouring Namibia and Western Zambia.’

In Cuando Cubango four municipalities (Calai, Cuangar, Dirico, Rivungo) with 14 population centres (Calai, Mapupu, Cambridge, Cuangar, Savate, Cahila, Kandendere, Dirico, Muccusso, Xamavera, Kangongo, Rivungo, Jamba, Bairro Nova) have been targeted for IRS. In Cunene 3 municipalities (Ombadja, Cuvelei, Namacunde) have been targeted with 10 population centers (Calueque, Naulila, Xangongo, Mukolongondjo, Calonga-Nampala, Cubati-Cachuea, Mupa, Namacunde, Santa Clara, Chede). See maps below.
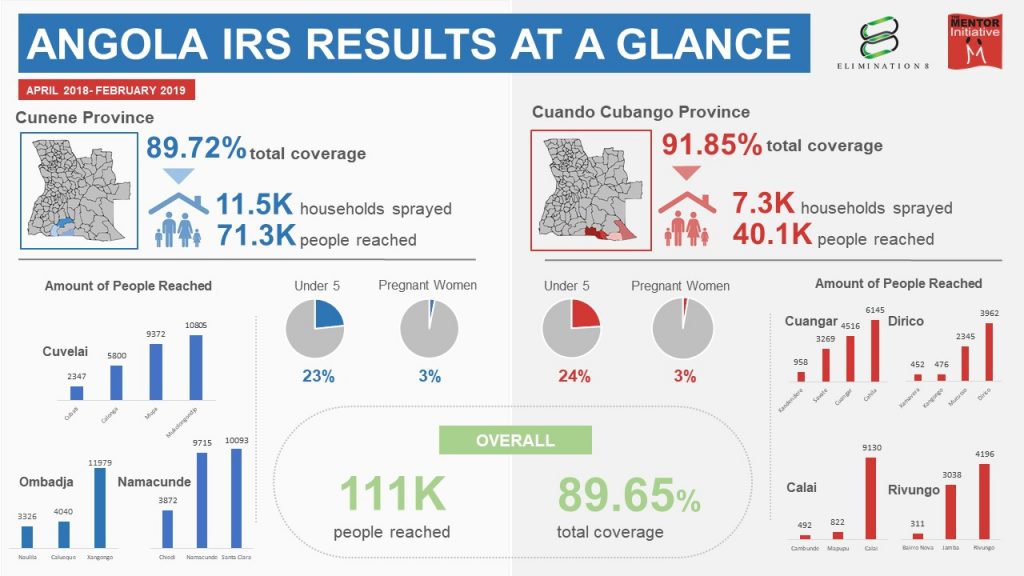
The program aimed to cover 85% of targeted houses but exceeded this aim with a total coverage of 89.65%. A total of 18,898 houses were sprayed with Actellic 300 CS © (Pirimiphos-methyl) out of the 21,079 identified in the target areas; protecting an overall population of 111,464 individuals from malaria. Of these individuals, 26,313 (24%) were children under 5 and 3,246 (3%) were pregnant women.
Key Results:
- In Cunene province, 71,349 people were protected from malaria in 11,512 out of 12,831 households through Indoor Residual Spraying, achieving a household coverage of 89.72%.
- In Cuando Cubango province, 40,115 people were protected from malaria in 7,386 out of 8,248 households through Indoor Residual Spraying, achieving a household coverage of 91.85%.
- In Cunene and Cuando Cubango, a total of 18,898 houses were sprayed out of 21,079 houses identified/visited in target areas, protecting an overall population of 111,464 individuals from malaria, achieving an overall household coverage rate of 89.65%.
- Of the 111,464 people protected by IRS in Cuando Cubango and Cunene, 23% (26,313) were Children under 5 years and 2.9 % (3246) were pregnant women.
Lessons Learned and Next Steps
Community mobilisation and buy-in during spray campaigns is important. Not achieving these can mean refusals from home owners to participate in the campaign or homes not being open during the campaign. This has an impact on coverage which affects the level of protection for that community. During the campaign at times the spray team met home owners who were reluctant to have their homes sprayed, due to fear of insecticide side effects amongst other reasons. In these cases, the teams would try to debunk any misconceptions. While refusals can be remedied in later IRS rounds, sufficient prior mobilisation is better. In fact, in some communities prior mobilisation saw neighbours convincing other reluctant members of the community of the benefits of spraying. Despite initital refusals, with intense mobilisation assisted by the community, public health directors and administrators MENTOR managed to achieve a total household coverage of 89%.
[Best_Wordpress_Gallery id=”10″ gal_title=”Angola IRS July 2019″]Furthermore, accurate baseline household data can be difficult to get but crucial in terms of quantity of materials needed and time allocated per area. Again, while MENTOR has the capacity and expertise to adapt to the reality of the situation during implementation in a particular community, our team will strive to continually have more accurate baselines prior to implementation by conducting necessary field assessments and consultations.
Working in southern Angola poses a logistical challenge, particularly in Cuando Cubango as road access was difficult. The roads are mostly sandy and lots of man hours were needed to move between field locations. Dealing with that, the challenges of car maintenance and frequent staff turnover in an area that is remote and isolated, proved difficult. To remedy this, staff were motivated and proper vehicle maintenance was ensured. In the end logistical challenges were overcome almost all targeted households were reached.

During 2018, data collected through surveillance border points showed significant reduction in malaria positivity rates in the areas where spraying took place compared to the same period in previous years.[3] This can partly be attributed to the spraying, partly to the combined efforts of several partners implementing surveillance approaches, and partly to the extended dry season which created an inhospitable environment for the mosquitoes. However, despite this reduction, further spraying is still necessary and there is still much work to be done in Angola to reduce the burden of malaria and to also stop cross border transmision into countries with elimination targets. Vector control along with surveillance, case management and community mobilization remain the most effective measures to prevent malaria transmission and ensure quick gains. Present gains in the reduction of malaria mortality and morbidity may be maintained as long as appropriate vector intervention strategies are sustained and adapted to understand and inhibit vector-related transmission dynamics .
[1] WHO 2018 Angola profile, https://www.who.int/malaria/publications/country-profiles/profile_ago_en.pdf?ua=1
[2] PMI 2019 Operational Plan https://www.pmi.gov/docs/default-source/default-document-library/malaria-operational-plans/fy19/fy-2019-angola-malaria-operational-plan.pdf?sfvrsn=3
[3] Trans Kunene Malaria Initiative surveillance border points data (2018 & 2019)